With the new year comes new goals of health and fitness for many people. Oftentimes with the start of a brand new exercise routine or a currently updated one, an onslaught of fresh aches and pains joins in on the fun. One of the most common complaints that walks through the door of our chiropractic and sports medicine office is the beloved shin splint. Too much too soon of a new activity easily results in irritation of the muscles, tendons and bones of the lower leg. For many people they will resolve on their own after the tissues get accustomed to the intensity of the activity. But when they don’t improve, it’s important to get evaluated to find out the underlying cause(s), address them, and keep the shin splints from ever returning or worse, progressing into a stress fracture.
Definition and Anatomy of Shin Splints
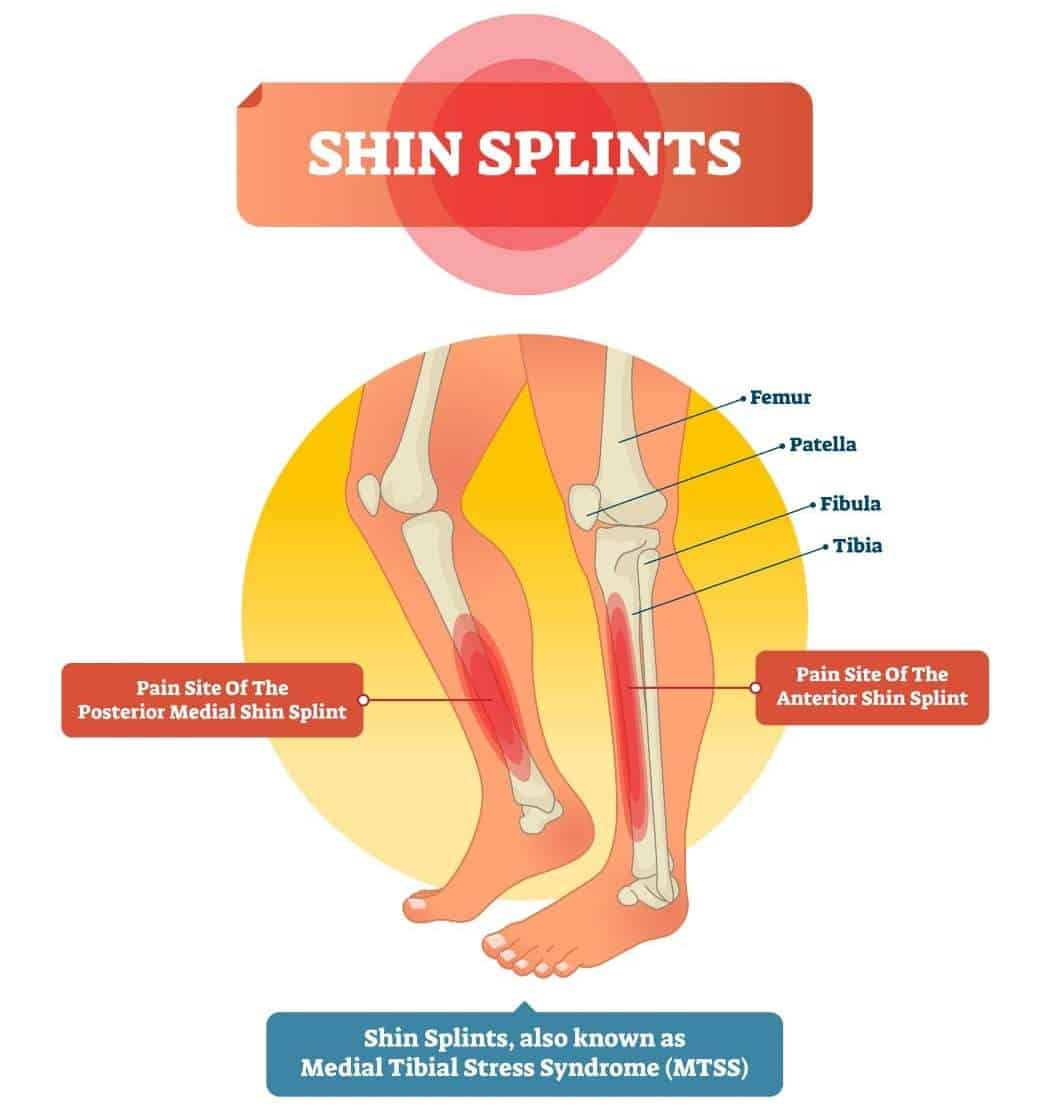
Shin splints can be defined as pain along the tibia due to repetitive stress of the surrounding soft tissue. The main types are medial and anterior based on the areas involved. Pain on the most lateral or outside of the shin isn’t considered a true shin splint by the medical profession but rather a tendinopathy of the peroneii muscles that live there.
- Medial shin splints are traditionally associated with issues of the Tibialis Posterior muscle. The TP originates on the back of the tibia and fibula then runs along the inside of the shin and attaches to multiple bones on the bottom of the foot.
- Anterior shin splints are traditionally associated with issues of the Tibialis Anterior muscle. The TA originates at the upper portion of the tibia and travels down the shin to attach to the top of the foot.
Alternative names for Shin Splints
Shin splints are often referred to using the following alternative terms and names:
- Medial Tibial Stress Syndrome (MTSS)
- Anterior Tibial Pain
- Exercise-Induced Leg Pain
- Tibial Periostitis
- Posterior Tibial Shin Splints
- Lower Leg Pain
- Traction Periostitis
- Periostitis of the Tibia
Common Causes of Shin Splint
Shin splints are common injuries in runners, dancers and athletes who do high impact activities. However, any person starting a new exercise activity or adding intensity to their workout regime is prone to developing shin splints.
- A sudden change in intensity or duration of an activity can easily anger muscles that aren’t used to the demand.
- Instability of the ankle joint.
- Poor footwear.
- Rough terrain can also contribute to shin splints.
- More often than not though, under performing muscles are the underlying cause of most repetitive stress injuries. More on that later.
When Should You See a Professional if You Experience Shin Splints: Consulting a Sports Chiropractor
It should be expected to experience new aches and pains at the beginning of any new workout routine.
- Wait 2 weeks after you experience the first symptoms of shin splints and apply at-home treatment.
My professional opinion is to give them at least 2 weeks to resolve on their own while continuing the training program. Sometimes things just need to acclimate to their new situation and will settle in. Gentle self-massage, and icing the area may manage the discomfort until then. - It’s time to contact a sports medicine practitioner or sports chiropractor and get checked out if:
- the pain in the lower leg does not improve during or after the activity,
- there is pain even at rest,
- the area is very tender to the touch or appears to have a bit of swelling.
Can a Sports Chiropractor Help with Shin Splints?
Most people wouldn’t think to go see a chiropractor for shin splint treatment and relief. But as Diplomats and Certified Sports Practitioners we have expanded our knowledge base way past just spinal complaints and adjustments. As sports chiropractors, we specialize in the care of musculoskeletal injuries and are well-versed in dealing with sports-related conditions like shin splints. Below you can find the comprehensive evaluation and treatment process for shin splints that we use in our Smithtown chiropractic office.
Shin Splints Treatment Protocol

Step 1. Shin Splint or Stress Fracture?
The first step that I take in the evaluation process is to rule out a stress fracture.
- Perform the hop test to rule out the stress fracture. This test involves the patient hopping on the affected side – but it’s not a gentle bounce. It’s a true jump with a hard landing on the entire foot base. A stress reaction or fracture will cause severe focal pain in the shin.
- Other tests include placing a tuning fork along the tibia or using ultrasound therapy. The vibratory effects of these tests are extremely painful if there is a break in the covering of the bone (periosteum) and is indicative of fracture.
In case of a positive test, we will refer the patient to the orthopedic doctor for further treatment.
If the results are negative, we move on to the next step: ankle mobility and muscle test.
Step 2. Ankle Mobility and Muscle Test
The next step includes evaluation of the ankle mobility and muscle test of all the distal leg musculature. Based on what I find to be weak determines what exercises will be given, obviously. Sometimes it’s as simple as the Tibialis Posterior being the under performing muscle, so TP activations will be assigned as homework.
However, it doesn’t always work out that way. I often find that the TP is strong but a muscle in the hip is actually weak and causing the TP to be overworked. This results in a TP overuse injury. In this case, the hip muscle has to be turned on and strengthened in order to give the TP a break.
Now remember, this is only one example, and one compensation pattern. There are so many ways that people compensate, and everyone is different. It’s our job to piece it together and then teach our patients how to fix the issue.
Two examples of muscles that are often found to be culprits in medial shin splints: ~a weak TP (Tibialis Posterior) ~a weak piriformis
Two examples of muscles that are often found to be culprits in anterior shin splints: ~a weak TA ~weak quads
Step 3. The Myofascial Work and Soft Tissue Release
I never just treat the one area that hurts. I hit all the surrounding areas with deep tissue release therapy, Graston or even cupping. I’ll also stretch the same areas. Using ultrasound to treat the specific injured muscle is also a possibility as well as taping. I prefer leukotape for shin splints, especially if I have to get somebody through an upcoming event, race or game. But please be aware, the manual therapy does not fix the issue alone. The body has to learn something in order to have a more permanent change. The exercises are what makes the true difference – not just getting rubbed and stretched.
Step 4. At-Home Exercise Protocol
The body has to learn something in order to have a more permanent change. The exercises are what makes the true difference – not just getting rubbed and stretched.
If a patient is diligent with their home exercises, within a week they should start to feel improvement in their symptoms. I really do try to fix people in one visit, but sometimes follow up visits are needed to weed out other underperforming muscles that are contributing to their injury. Assigning too many exercises at once results in sensory overload and doesn’t allow for full learning potential, so I try to keep the amount of exercises I prescribe to only 1 or 2 per session. If I do my job properly and my patients do their part, they will be back to full sport within 2 weeks.
How to Prevent Shin Splints
For people who aren’t already patients of ours but want to try to prevent shin splints, I advise checking out our YouTube channel. Get acquainted with the activations for the TA, TP, peroneii, gastroc and soleus muscles. Learning how to properly connect to these major players of the lower leg could absolutely make a positive difference in prevention of injury and in performance. Whenever possible, performing exercises unilaterally improves their efficacy. One side at a time is the best way to maximize results.
Recommended Rehabilitation Videos for Shin Splints
Tibialis Posterior Activation
Tibialis Anterior Activation
Peroneii Activation
Soleus Activation
Gastrocnemius Activation
Piriformis Activation
Foot Drills
Quads Activation
Please consider us when dealing with any of your musculoskeletal complaints, not just neck or back. We quickly figure out what the issue is, why it happened, treat it and teach you how to handle it. You’ll be educated in how to treat yourself and have video references in case you forget. We want our patients to walk away from their experience with us feeling like they’ve been heard, learned something that has been specifically tailored to help them and that they can be proactive about their current and future injury care and prevention.
References
- Bhusari, N., & Deshmukh, M. (2023). Shin Splint: A Review. Cureus, 15(1). doi:10.7759/cureus.33905
- Deshmukh, N. S., & Phansopkar, P. (2022). Medial Tibial Stress Syndrome: A Review Article. Cureus, 14(7). doi:10.7759/cureus.26641
- MedlinePlus Medical Encyclopedia. (2023). Shin splints – self-care. Online publication.










