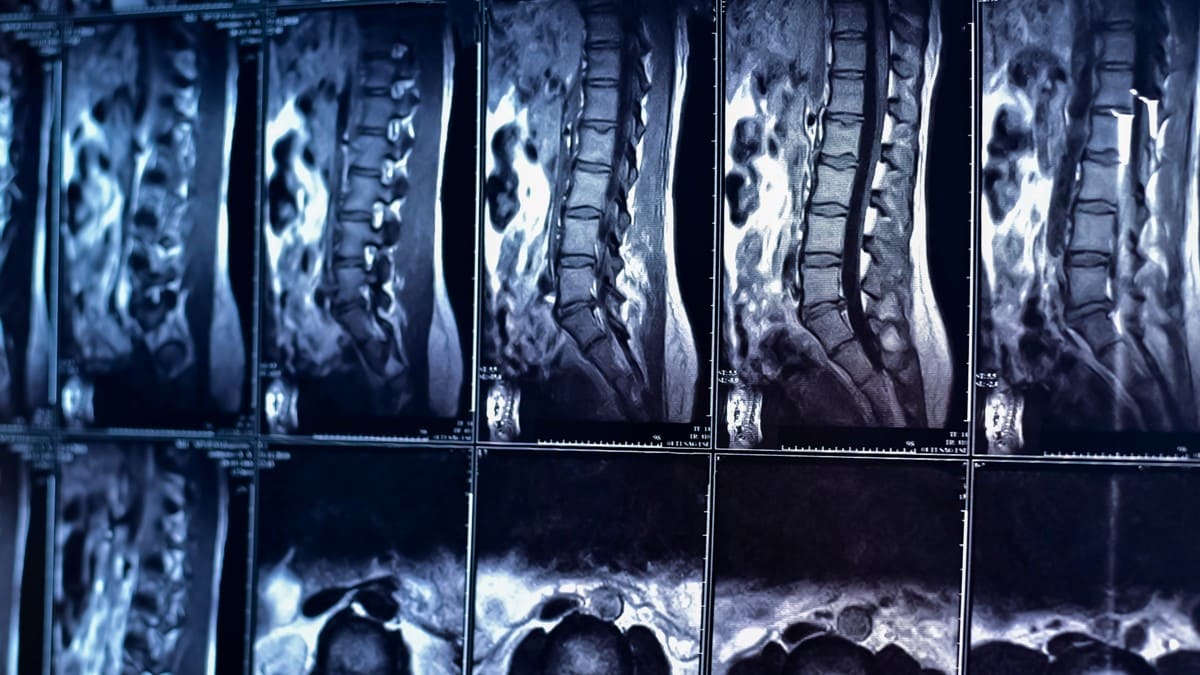
When you’re in pain, it’s natural to want answers – fast. For many people dealing with lower back pain, an MRI seems like the obvious next step. After all, it’s a powerful imaging tool that can reveal the intricate details of your spine, right? But what if I told you that an MRI, while valuable, might not always be the best first step in diagnosing your back pain?
In my years of practice, I’ve seen countless patients who come in with their MRI results, anxious about the findings and worried about what they mean for their future. However, the truth is that these images are just one piece of a much larger puzzle. They can show us structural abnormalities, but they don’t always tell the whole story.
Before you pin your hopes – or your fears – on what an MRI reveals, it’s important to understand the broader context of back pain diagnosis. Let’s explore why an MRI isn’t always the answer and how a more comprehensive approach can often lead to better outcomes.

What is an MRI?
Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic tool that uses powerful magnets and radio waves to create detailed images of the inside of your body. Unlike X-rays, which are great for viewing bones, MRIs are particularly effective at imaging soft tissues, such as muscles, ligaments, and discs in your spine. This makes MRI a go-to method for identifying structural issues like herniated discs, spinal stenosis, and other abnormalities that could be causing back pain.
My Journey with Back Pain and MRI
From my 30’s, I had a history of low back pain. It was manageable for the most part but it would occasionally crescendo and require treatment. After adjustments, massage, acupuncture, etc, I’d be back in business.
I remember pretending to be an Olympic lifter in the gym and began exercises associated with these lifts. Hang cleans, power cleans, snatches, etc. It was then, I believe, that I exacerbated my spinal complaint. I felt numbness and tingling in my right leg. I started to feel uncomfortable at night and had to bolster myself in such a way as to avoid the leg pain.
One January (circa 2007) we were at the St. James Chamber of Commerce Winter Gala. Dancing, drinking, and eating were essentially the activities. That night, no matter how I bolstered, I could not get comfortable. I asked Hope to take me to the ER due to my level of pain. I was given five days worth of a fantastic cocktail of Prednisone, Oxy, and a muscle relaxer, and did I ever sleep well. It knocked the pain down a ton, but it didn’t solve my issue.
After a few frustrating weeks of sleeping in a recliner with heat and stim (electrical stimulation therapy) which only offered interrupted sleep, I decided to visit a pain management ortho who ordered an MRI.
You name the finding and I had it. Stenosis, bulging, herniations, etc. (Quick aside – As I was typing this, I must have misspelled bulging, and it spell-corrected to balding! DO NOT LAUGH AT THAT.) He recommended epidural injections. A course of 3 injections, each being 2 weeks apart, was the protocol back then. Not the most comfortable treatment, but I was willing to try anything. The third injection really did the trick. My pain reduced enough so that I could really work hard and improve my spinal situation.
Epidural injections do not fix stenosis. They don’t fix bulging or herniations either. So why did my symptoms resolve? My nerve at the level of the herniation or bulge was irritated and inflamed. The medicine which was injected into the spinal nerve area reduced the inflammation on the nerve. The structure was essentially unchanged. I dove deep into rehabilitation and core work. I was a very PROACTIVE patient.
15 years later and I don’t consider myself a back patient. I know my MRI will likely look worse than it did back then, but I’m not concerned because I’m asymptomatic. Too many people get an image done and see that there are findings. That then becomes their default response to any discomfort in their spine. In fact, I’ve even heard a patient explain that they feel their disc “slip.” In my opinion, that is highly unlikely.

When MRI Results Don’t Tell the Full Story: A Powerlifter’s Experience
Another story about structure vs. function. We had a powerlifter (masters champion) who complained of knee pain. He wasn’t responding in 2-3 treatments so we ordered the MRI. We saw the results and in my opinion I was going to be giving him the bad news that his lifting was probably over. Every bad kind of finding. He came in on the next visit and I asked, “How are you feeling?” He said he felt pretty good and squatted 450lbs. I essentially took the MRI and threw it in the garbage. Not really, but I did explain to him that although his MRI findings weren’t great, he should simply continue to do what he was doing.
Why MRI Isn’t Always the Answer
While MRI is a powerful diagnostic tool, it’s not always the best – or first – step in diagnosing back pain. Here’s why:
- Overemphasis on Structural Abnormalities: MRI scans can reveal detailed images of your spine, including herniated discs, bulging discs, or spinal stenosis. However, not every abnormality found on an MRI is necessarily the cause of your pain. In fact, studies show that many people with these findings on an MRI are completely pain-free. This can lead to unnecessary anxiety and even unnecessary treatments.
- Lack of Functional Insight: MRI provides a static image of your spine, but it doesn’t capture how your body moves or how your muscles and nerves function. Back pain is often related to functional issues – like muscle imbalances, weakness, or improper movement patterns – that MRIs simply can’t detect. This is why a comprehensive physical assessment when diagnosing back pain is crucial.
- Potential for Overuse: Because an MRI can be so revealing, it’s sometimes overused, leading to a “more is better” approach. But in reality, jumping straight to an MRI can result in a misdiagnosis, overtreatment, or overlooking the real cause of the pain.

Our Approach to Diagnosing and Treating Back Pain
At True Sport Care and Chiropractic, for low back pain or really any pain, we focus on finding and fixing the root cause of your pain. Here’s how we do it:
Step 1: Assessing Weaknesses and Imbalances
We start with a thorough assessment to identify any weaknesses, imbalances, or asymmetries in your body. This helps us understand what’s really causing your pain.
Step 2: Targeted Exercises
Next, we guide you through targeted exercises to strengthen and correct these issues, one muscle group at a time. Our goal is to address the problem at its source, not just mask the symptoms.
Step 3: Soft Tissue Work and Chiropractic Adjustments
We use soft tissue techniques to reduce muscle spasms and trigger points, and perform chiropractic adjustments to correct any spinal misalignments. This comprehensive approach helps alleviate pain and restore proper function.
Step 4: Weekly Check-ins
We check in with you weekly to monitor your progress. In many cases, symptoms resolve before we even consider imaging.
Step 5: Imaging and MD Collaboration
If someone doesn’t respond in the first few sessions, we then grab an image to see if there’s a good reason why they aren’t responding. We also send patients to MDs when they do not respond. Sometimes we need to break the pain cycle and prescription meds help with this. We’ve even had some scenarios when we didn’t wait (more on that below.)
When To Get an MRI and/or Immediate Medical Attention
One patient who was an extremely sturdy elderly gentleman came in. We hadn’t seen him in a while, but he typically ambulates well on his own. He was on a walker and I asked, “What happened?!” He said his legs kinda stopped working. We got him in with a spinal ortho ASAP and he had surgery within that week. A synovial cyst was pressing on his nerve.
Here is when we recommend our patient to get an MRI for their back pain complaints:
Unexplained Muscular Weakness or Other Neurological Deficits
Numbness, tingling, burning, aching and pain are considered sensation symptoms. Even though they may suck, they often don’t affect your function. Muscle weakness, especially weakness without pain, is the more concerning symptom. Other warning signs include loss of reflexes or sensory changes. Our antennae definitely go up on these patients. This does affect function and whenever we have a patient who presents us with a low back (or neck) complaint with unexplained weakness, we don’t hesitate to send them to an MD so we can co-manage their case.
Low Back Pain in Kids and Young Athletes
Other times when our radar goes up is in the case of a pre-skeletally mature athlete who complains of low back pain. Additionally, if they participate in a sport which requires extension and rotation, then we are on guard. There are certain tests that can be done, but an MRI is warranted early on to diagnose a Spondylolysis.(weakness or stress fracture in one of the vertebrae).
No Improvement in Symptoms after 6-8 Weeks
If we don’t see any improvement in your symptoms in 6-8 weeks then we would recommend an MRI. In reality, we don’t believe in dragging out treatment without progress. We stand by our 3-visit guarantee:if your issue doesn’t resolve or show significant improvement within three visits, we’ll refer you to a different professional who can help. We will refer you to imaging or a different professional way before the 6-week rule. However, if you are reading this article and are going through conventional back pain treatments elsewhere, you should seek a different opinion and an MRI if your pain is not getting better after 6-8 weeks.
Suspected Spinal Tumors or Infections
We usually don’t see patients in our chiropractic office who present with the symptoms of these conditions but, for the sake of the completeness of this article, I must mention these important indications for an MRI.

Trust More Than Just the MRI
An MRI can show you a lot, but it doesn’t always tell the whole story. It’s just one tool in the toolbox. At True Sport Care and Chiropractic, we know that back pain isn’t just about what you see on a scan – it’s about how your body feels and moves (or “function over structure” as we frequently emphasize in our articles and when communicating with our patients). That’s why we focus on the big picture, combining hands-on treatment, targeted exercises, and, when needed, imaging to get you back to feeling your best.
If your back pain isn’t getting better, don’t wait around. If you are located on Long Island, give our office a call and let’s find and treat the true source of your pain together. You deserve more than just a diagnosis – you deserve a solution.
Resources
- Brinjikji, W., et al. (2015). Imaging strategies for low-back pain: systematic review and meta-analysis. The Lancet, 384(9946), 463-472.
- Atlas, S. J., & Deyo, R. A. (2001). Evaluating and managing acute low back pain in the primary care setting. Journal of General Internal Medicine, 16(2), 120–131.
- Jarvik, J. G., & Deyo, R. A. (2002). Diagnostic evaluation of low back pain with emphasis on imaging. American Journal of Roentgenology , 179(3), 601–608.
- Flynn, T., Smith, B., & Chou, R. (2011). Appropriate use of diagnostic imaging in low back pain: A reminder that unnecessary imaging may do as much harm as good. Journal of Orthopaedic & Sports Physical Therapy, 41(11), 838–846.
- Davis, M. A., Belk, K. L., & Mahomed, K. (2020). Trends in the diagnosis and treatment of lumbar spine conditions in the United States. The Journal of the American Board of Family Medicine, 33(6), 842–850.
- Knezevic, N. N., Mandalia, S., Raasch, J., Knezevic, I., Candido, K. D., & McCormick, Z. (2018). Treatment of chronic low back pain – new approaches on the horizon. Journal of Pain Research, 11, 1111–1123.