Plantar fasciitis is one of the most common causes of heel pain, affecting millions of people worldwide. The condition occurs when the plantar fascia, a thick band of tissue running across the bottom of the foot, becomes inflamed or irritated. This inflammation typically results in stabbing pain near the heel, especially during the first steps of the day or after periods of inactivity.
What Causes Plantar Fasciitis?
The plantar fascia supports the arch of the foot and acts as a shock absorber as we walk or run. Overuse, strain, or stress on this tissue can result in micro-tears, leading to inflammation and pain. There are several contributing factors to the development of plantar fasciitis:
- Age: Plantar fasciitis is most common but not limited to people between the ages of 40-60.
- Activity levels: Athletes, especially runners or individuals who engage in high-impact sports, are at higher risk. Sudden increases in activity intensity or duration can also trigger the condition.
- Obesity: Hate to say it but excess weight puts additional pressure on the plantar fascia, increasing the likelihood of inflammation.
- Foot mechanics: Individuals with flat feet, high arches, or abnormal walking patterns (pronators or supinators) are more susceptible due to altered weight distribution.
- Occupational risks: Jobs that require standing or walking on hard surfaces for extended periods of time can lead to the condition.
Anatomy of the Plantar Fascia
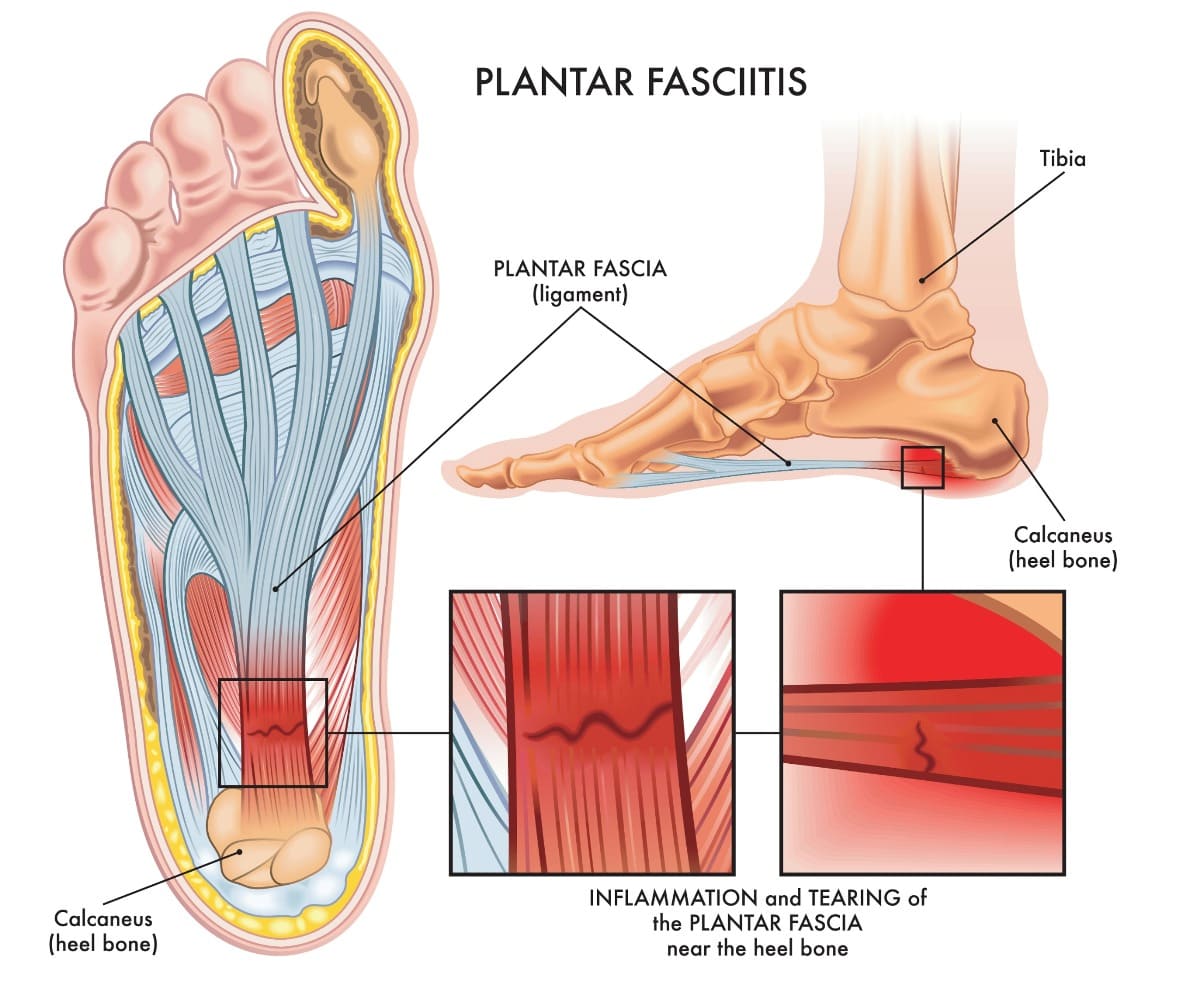
The plantar fascia or plantar aponeurosis is a long thin fibrous band that extends from the heel to the digits on the plantar or underside of the foot. The plantar fascia is of great strength and supports the arch. It is divided into three portions.
- The thickest is the central portion which attaches to the medial process of the tuberosity of the calcaneus.
- The lateral and medial portions cover the sides of the sole of the foot. The lateral portion is thick where it radiates from the central portion, then this as it stretches longitudinally toward the first metatarsal or pinky toe.
- The medial portion also radiates from the central portion but is thinner and covers the under surface of the abductor hallucis muscle which moves the great toe.
Plantar fasciitis is a condition in which plantar fascia gets inflamed or irritated. If left untreated, it can lead to plantar fascia tears.
Plantar Fasciitis Prevalence and Stats
Plantar fasciitis is prevalent across various populations:
- US: it is estimated that about 2 million people are treated each year.
- Studies suggest that up to 10% of the population will experience plantar fasciitis at some point in their lives.
- A 2019 study in the journal Foot and Ankle International found that plantar fasciitis accounts for approximately 8% of all running injuries, making it a common concern for athletes.
- Occupational studies have shown that individuals working in physically demanding jobs report a 15-20% prevalence of heel pain, with plantar fasciitis being a significant contributing factor.
Symptoms of Plantar Fasciitis
The hallmark symptom of plantar fasciitis is sharp, stabbing pain in the heel or arch, typically felt in the morning or after long periods of sitting or standing. The pain may lessen throughout the day but can worsen after extended physical activity or standing on hard surfaces. Additional symptoms include:
- stiffness along the bottom of the foot
- swelling or redness
- pain after exercise (typically not during)
Diagnosis
Plantar fasciitis is usually diagnosed via medical history and physical evaluation. Key signs include tenderness to touch in the heel and bottom of the foot along with pain and tightness with dorsiflexion. If conservative care doesn’t make a significant impact, further diagnostic testing like X-rays or MRI’s may be utilized to rule out more ominous conditions like stress fractures or more damaging soft tissue injuries.
Plantar Fasciitis Treatment and Management

Most cases of plantar fasciitis can be managed with conservative care, if the patient is willing to put in a little effort and change their way of thinking.
- Activity modification: we don’t like to tell patients to stop being active, so reducing, modifying, or replacing the offending activity is often advised until we can get the situation under control.
- Myofascial work – in the office we use myofascial release to help soothe the pain associated with plantar fasciitis. Myofascial release can be applied to both plantar fascia and calf muscles to help release the restrictions and tightness in this area. Simple myofascial release techniques can also be performed at home, for example rolling out of the feet using a tennis or golf ball.
- Joint manipulation of the toes, foot and ankle. Chiropractic adjustment to the foot and ankle joints will take the pressure off the plantar fascia allowing it to release. The adjustment will also improve the mobility and function of the joints which are commonly compromised in patients with plantar fasciitis.
- Ultrasound therapy for plantar fasciitis improves blood flow and circulation to the damaged area, bringing in more oxygen and nutrients. This jumpstarts a healing response from your body and reduces swelling and inflammation.
- Strengthening exercises for underperforming musculature is the key for taking care of this issue. The plantar fascia often takes the brunt of muscles that don’t work the way they should and winds up with an overuse injury. I can’t tell you how many people use their calves, feet, and toes to fire their quads or glutes or lower back extensors etc. That poor plantar fascia never gets a break. It’s so important to figure out why it’s happening so that patients can learn how to fix it, maintain the proper mechanics and avoid it from returning.
- Stretching protocols for calves and the Achilles tendon. Tight muscles in the calf (gastrocnemius and soleus) and foot can aggravate pain associated with plantar fasciitis. However, we can’t stress enough the importance of addressing the ROOT cause of the pain complaint which is often weakness of one of the muscles along the chain. Stretching will provide temporary relief but strengthening the underperforming/ disconnected muscles is what will keep plantar fasciitis from reoccurring.
- Footwear: Supportive shoes with proper cushioning and support can reduce pressure on the plantar fascia.
- OTC Anti-inflammatories: sometimes a little extra help is necessary to reduce pain and inflammation.
- Steroid injections: we don’t recommend this route. It usually gives only mild relief of symptoms and doesn’t permanently fix the issue. In addition, steroid use can weaken and damage the tissues we’re trying to help.
- Surgical intervention: this should be avoided if possible. Oftentimes surgery winds up causing more problems that cannot be reversed.
True Sport Care and Chiropractic Approach to Treating Plantar Fasciitis
In our Smithtown chiropractic and sport medicine office, we use an effective approach to treating plantar fasciitis that is different from the traditional treatments. In the video above, Dr. Marc Taczanowski discusses how our doctors can reverse the dysfunction quickly and permanently. The key to our success in treating plantar fasciitis lies in focusing on the whole body rather than just the spot where the pain presents itself. Pain is typically a distraction and when a practitioner ONLY treats the site of pain, they are usually unsuccessful.
There are many muscles that can be involved in the mechanism of muscular dysfunction that leads to foot and heel pain. We perform a thorough evaluation and assessment to find the muscular imbalances that contribute to the condition. Our treatment plan for plantar fasciitis includes therapeutic exercises that correct the muscular imbalances discovered during the assessment as well as manual therapies designed to relieve heel/foot pain, reduce inflammation of the fascia as well as promote healing in the area.
Will Stretching be Enough to Treat Plantar Fasciitis?
There are many muscles that can be involved in the mechanism of muscular dysfunction that leads to foot and heel pain. The most common denominator in a plantar fasciitis mechanism is tight calves.
Does it mean that stretching would be sufficient to treat the plantar fasciitis pain and avoid it in the future? Not really.
A tight muscle doesn’t become tight arbitrarily. There must be some GOOD reason for its tightness. When testing out the muscles of the posterior chain, we often see tight calf muscles but this is not the full story. What do we always look for? The WEAK structures.
The weak structures promote other normally functioning (often in the same chain) muscles to work harder. That extra stress begins to exceed the muscle load capacity causing tightness. When talking about plantar fasciitis and tight calves, the usual culprits are disconnected glutes, and hamstrings. See that I didn’t use the word weak. Not the best description. People usually say, “I work my glutes, I work my hamstrings, I do the exercises I saw in Runners World magazine.” You can do the same exact exercises perfectly and still work around a disconnected muscle. Unless this disconnection is addressed, you will not be able to correct the movement patterns. And, in turn, no amount of stretching of the calves will be sufficient to keep the calves from getting tight and pulling on the plantar fascia and causing more foot pain in the future.
I can’t stress this enough. Don’t guess where the problem may be stemming from. If you are located on Long Island, get tested by any of our expert chiropractors and sports medicine practitioners and learn where your disconnect may be so that you can successfully treat plantar fasciitis pain.

How Long Does it Take to See Improvement in Plantar Fasciitis?
Most patients with plantar fasciitis recover with typical conservative care within 6-12 months. With our highly specialized muscular evaluation and type of treatment, we see improvement within a week or two. Early intervention is key in preventing chronic pain and long-term complications-so get checked out sooner than later.
Plantar fasciitis is a common but manageable condition that can significantly impact daily life, particularly for those with high physical activity levels or certain occupational risks. With proper treatment and preventative care, most individuals can expect full recovery and return to their normal activities without long-term consequences. Early intervention and consistent management strategies are key to reducing the discomfort associated with this painful condition.
References:
- Frey C, Zamora J. The effects of obesity on orthopedic foot and ankle pathology. Foot Ankle Int. 2007 Sep.
- Knobloch K, Yoon U, Vogt PM. Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int. 2008 Jul.
- Çil ET, Şaylı U, Subaşı F. Outpatient vs Home Management Protocol Results for Plantar Fasciitis. Foot Ankle Int. 2019 Nov.
- Arif MA, Hafeez S. Effectiveness of Gastrocnemius-Soleus Stretching Program as a Therapeutic Treatment of Plantar Fasciitis. Cureus. 2022 Feb.
- Yelverton C, Rama S, Zipfel B. Manual therapy interventions in the treatment of plantar fasciitis: A comparison of three approaches. Health SA. 2019 Sep.
- Russo L, Montagnani E, Pietrantuono D, D’Angona F, Fratini T, Di Giminiani R, Palermi S, Ceccarini F, Migliaccio GM, Lupu E, Padulo J. Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour. Int J Environ Res Public Health. 2023.
- Ajimsha MS, Binsu D, Chithra S. Effectiveness of myofascial release in the management of plantar heel pain: a randomized controlled trial. Foot (Edinb). 2014 Jun.



